Volume Management
There are many factors that can affect volume of a residual limb.
Muscle atrophy, weight changes, diet, medication, and increased or decreased physical activity can all have significant effects. Managing these volume changes is important to ensure a well-fitting socket, which will increase stability and comfort when walking.
- After amputation surgery, we encourage our patients to wear a shrinker for about 2 weeks prior to casting. This helps to reduce postoperative edema (swelling) in the residual limb and will aid in shaping the limb for comfortable prosthetic fitting. Elevating the limb will also help to reduce swelling.
- After delivery of the prosthesis, we still want to manage volume as it can change from day to day, from morning to afternoon, and even from hour to hour. Socks are an excellent way to maintain a snug fit in your prosthesis.
- If you experience significant volume changes from day to day, keep a log of your diet and medications to show to your physician. Eating a salty meal will cause your body to retain water, which could increase volume in your residual limb. Certain medications can cause your body to increase or decrease water retention as well.
- Dialysis can have a significant affect on residual limb volume. Make sure your prosthetist is aware of when and how often you have dialysis as this can affect fitting of a prosthesis.
- Increased physical activity will most likely reduce your volume. When you put weight on your prosthesis, there is a pumping action of the muscles that will push the fluid out of your limb. You will most likely need to add socks if you are doing a significant amount of walking or going to the gym.
- Sitting with your leg hanging off a chair will increase volume. If you are sitting, elevate your limb to prevent fluid collection.
- Weather can affect volume as well. Heat can cause increased swelling, and high or low-pressure systems accompanying storms can affect your limb as well, affecting volume and sometimes increasing phantom limb type sensations.
If you are concerned about volume fluctuations or feel like adjustments need to be made to your prosthesis, call your prosthetist for an appointment.
Sweat
“How do I stop sweating so much?”
This is one of the questions we hear most often from our amputees.
Unfortunately, sweat is something that, to a certain degree, is going to happen no matter what. Most liners are made of a gel material, which retains heat and will not wick moisture away from your limb.
Excess sweat can cause several issues when using a prosthesis.
First, excess sweat can cause friction between your liner and your skin, which could lead to the formation of blisters. Blisters can take a long time to heal, and if they burst can become infected.
If blisters or other skin breakdown occurs, your physician or prosthetist may suggest not wearing the prosthesis and staying off your feet for a few days to allow it to heal.
Secondly, excessive sweat buildup in the liner can cause the liner to slide on the skin.
This can affect suspension on your leg, and can cause shear forces which can lead to skin breakdown. Luckily, there are a few tips and tricks to managing and reducing the effects of sweat on your residual limb.
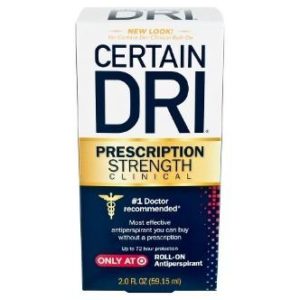
Antiperspirants — There is a specific antiperspirant that we have found works very well for our patients called Certain Dri. It can be found in most drug stores and does not require a prescription.
The important thing to remember when searching is to find an antiperspirant, not a deodorant. We typically suggest that our patients put Certain Dri on their limb at night after taking the liner off and cleaning their leg. After about 2 weeks of using this, our patients are typically seeing a dramatic reduction in sweat.
Note: start on a small section of skin first to ensure that you will not have any adverse reactions.
Liner liner — This is a very thin sock that goes between your leg and your liner. It will help to wick away moisture and reduce shear forces, which could cause skin breakdown.
Most liner liners will have silver fibers to help eliminate odors as well.
Suspension — There are certain types of suspension that can help reduce sweating, specifically vacuum suspension.
An active pump in the prosthesis maintains negative pressure in the socket, meaning the limb will always be in close contact with the gel liner, preventing sweat glands from generating excessive moisture.
What NOT to do
It is easy to be tempted to put baby powder or talc powder inside the liner to help absorb moisture.
However, the powder will just absorb the sweat and become a sticky paste inside the liner, making it uncomfortable and difficult to clean out. Additionally, using lotion before putting the liner on can increase the detrimental effects of sweat, such as skin breakdown or causing the liner to slide down your leg.
We typically encourage people to use lotion at night after cleaning their leg to allow time for the lotion to absorb into the skin. If you use lotion, use a non-scented lotion that is gentle on skin. Scented lotions can easily cause skin irritation, especially inside a hot and sweaty liner.
If you feel like you are having an issue with sweat, try these tips or speak to your prosthetist to find a solution specific to your needs.
Types of Knee Braces - Reduce Knee Pain & Prevent Injury
Types of Knee Braces
There are several different types of knee braces that range from simple compression sleeves to corrective braces. Based on the issues that you are having, your doctor or orthotist may suggest one of the following braces to be worn during certain activities or at all times.
- Functional Knee Braces: This is a type of brace that provides support to a previously injured knee. Oftentimes athletes will wear them after an injury has healed in order to stabilize the knee, control motion, and prevent further injury.
- Rehabilitative Braces: After surgery, this type of brace may be worn for several weeks to keep the knee stable but still allow some movement while the knee is healing.
- Unloader Braces: These are typically recommended for patients with knee osteoarthritis. (http://www.healthline.com/health/osteoarthritis/knee-arthritis-symptoms) brace acts to shift the weight from the damaged area of the knee, unloading it and reducing pain while you are walking.(https://www.verywell.com/what-is-an-unloader-knee-brace-2552051)
- Prophylactic Braces: These are designed to be used during specific activities, especially in contact sports such as football, to protect the knee from lateral or twisting forces.
- Knee Sleeves: While these are not technically braces, they are often prescribed as a compressive support for the knee joint. This helps to support the knee and can control pain and swelling in the joint. (https://breakingmuscle.com/fitness/the-advantages-of-knee-sleeves-what-they-are-and-when-to-wear-them)
How to Reduce Pain & Prevent Further Injury
When worn correctly, these braces have the ability to reduce pain and prevent further injury. However, there are a few common complaints that we receive with knee braces. Most of these issues have simple solutions.
- “My brace keeps falling down when I walk.”
- Since most people have a larger thigh and smaller calf, the conical shape of the leg itself allows the brace to migrate down the leg when you walk. You can try tightening the strap around your calf or try wearing something under the brace such as an ACE Some bandage or a sleeve such as Bracesox. Some braces also have adjustable metal uprights that your orthotist can contour to more intimately fit on your leg.
- “The side of my knee is red after I take the brace off.”
- Most often, we get this complaint from patients wearing an unloader style brace. This is because this style brace is providing correction to your leg and preventing it from going into the misaligned position it wants to be in. This is normal in this type of brace. Some redness is okay, but if it lasts more than 30-40 minutes or you begin to have skin breakdown caused by the brace, call your orthotist for an adjustment.
It is important to remember that while knee braces are an important part of recovery and prevention of injury, it is also important to maintain strength and flexibility in the muscles and tendons around your knee to reduce your risk of future injury.
Charcot Deformity
Charcot Deformity
The underlying cause of charcot foot (also commonly called charcot arthropathy or neurogenic arthropathy) is neuropathy. Since patients with neuropathy have a loss of sensation in their feet, they cannot feel the pain that accompanies the breakdown of the bones in their feet (http://www.footankleinstitute.com/charcot-foot-collapse).
Charcot is characterized by fractures and dislocation of bones and joints that occur with minimal or no trauma. The earliest sign of charcot deformity is a sudden or unexpected change in the appearance of the foot or ankle.
There is also typically accompanying redness, swelling, and heat.
This deformity most commonly affects the midfoot, but can also affect the hind foot, forefoot, and ankle. We see this deformity in some of our diabetic patients since diabetes causes neuropathy and loss of circulation in the feet. Loss of circulation can lead to resorption of bone, which weakens the bone and increases susceptibility to further fracture and dislocation.
Stages of Charcot Deformity
There are 3 general stages of charcot deformity:
- Stage 1 is considered the acute stage. In this stage, there is redness, swelling, and warmth in the foot. X-rays may reveal soft tissue swelling. Fractures and joint dislocation may be seen several weeks after the onset of this stage.
- Stage 2 is the subacute phase. Patients will experience decreased redness, swelling, and warmth, and X-rays will show some early healing of the fractures.
- Stage 3 is the chronic stage, characterized by reconstruction and consolidation of the bones. A deformity is often present, typically as a collapsed arch with rocker bottom deformity. Redness, swelling, and warmth have resolved.
Severe charcot deformities are typically referred to as a “rocker bottom foot” deformity, and can also be accompanied by an ulcer on the bottom of the midfoot. Ulcers are caused by excessive bony pressures against the shoe or ground.
The goals of treatment are primarily to protect the foot.; typical treatment includes unweighting the foot or distributing pressures over the bottom of the foot to allow healing, as well as to slow or stop the progression of bony breakdown.
In early stages, doctors may recommend total contact casts for 3-5 weeks to prevent micro-fractures from occurring in the bones of the foot. In later stages when the significant deformity is present, doctors may suggest a custom CROW or OWL boot. (http://www.podiatrytoday.com/article/2694) (http://www.orthomerica.com/owls)
Total contact boots that offload the bottom of the foot and prevent excessive motion of the foot and ankle when you are walking, which will slow development of further deformity.
Charcot foot and ankle can recur or flare up over time, and regularly occurs in both feet. Impairment and deformity resulting from charcot foot are permanent. If you have charcot, it is recommended that you use protective footwear or a custom boot any time you are walking or standing, as well as maintain regular follow up appointments with a specialist that can monitor your feet. This will help prevent further breakdown or deformity.
Diabetic Foot Care Tips
Diabetic Foot Care Tips
Two of the most important things you can do if you are diabetic are: control your sugar and take care of your feet. Diabetes can cause a loss of sensation in your feet, which means you could step on something or a callus could form and you wouldn’t know unless you take the time to look at your feet. It can also cause limited blood flow, which complicates and lengthens the healing process. People with diabetes also may have poor immune systems and can be more susceptible to infections. Left unchecked, calluses and injuries can lead to infected ulcers and ultimately to amputation. The good news is that amputation can be prevented by following these foot care tips.
- Check your feet daily: At the end of the day when you take your shoes off, inspect your feet. (http://www.webmd.com/diabetes/video/kahn-diabetes-patients-must-check-feet) you are not able to see the bottom of your feet, use a handled mirror. If you see any skin breakdown, including blisters or ulcers, stay off your feet and make an appointment to see your doctor. Continuing to walk on even small injuries can lead to larger injuries and wounds that are difficult to heal
- Early treatment: if you discover a wound on the bottom of your foot, see a doctor immediately to check for infection. If there is an infection, treatment with antibiotics is typically successful in early stages. If you continue to wait and walk on the wound, the infection could worsen and cause gangrene or bone infection.
- Wear proper shoes and footwear: Diabetic shoes are extra deep and extra wide to protect your feet from pressure, and don’t have seams on the inside that cause friction. They also allow room for diabetic foot orthoses, which distribute pressure over the entire foot, preventing pressure points that may lead to skin breakdown. It is also a good idea to wear seamless, padded, moisture-wicking socks. (https://www.drcomfort.com/our-footwear)
- Charcot: if you notice the shape of your arches changing, along with heat and redness at the arch, you may have a condition called Charcot, in which the bones of your feet break down. Left untreated, this can cause major deformity, which may lead to skin breakdown. (https://www.youtube.com/watch?v=e9p-Ql3pzYM) If you experience these symptoms, set up an appointment with your doctor. They may recommend that you get a brace to help support your arch and prevent further breakdown and deformity.
- Keep your skin dry: infections thrive in moist environments, so allow your shoes to air out and wear socks that wick away moisture.
- Avoid going barefoot: wearing shoes will help prevent you from stepping on debris or getting small cuts and scrapes on your feet that could lead to infection.
- Keep your nails clean and short: A fungal infection causes thickening of the toenails, and pressure on the top of the nail could lead to ulcers underneath, which are difficult to spot and treat and may lead to infection. (https://www.healthstatus.com/health_blog/diabetes-3/diabetic-nail-care/)
- Be careful of water temperature: when taking a bath, check the water temperature with your arm before stepping in. If you have loss of sensation in your feet, it’s easy to step into a bath and not realize you are actually burning your skin, which could leave you susceptible to infection.
If you are diabetic, it is extremely important to follow these tips to stay healthy and prevent any complications. Get into a regular routine of non-impact exercise, stop smoking, keep your sugar controlled, and get regular check-ups.
Knee Ligament Injuries - PCL, LCL, MCL & ACL Injuries
Common Injuries of a Runner
- Runner’s knee: A common overuse injury that results from the kneecap being out of alignment. Often, the cartilage on the kneecap wears down and can cause pain, particularly when going up or down stairs, squatting, or sitting with the knee bent for extended periods of time.
- Stress fractures: These are small cracks in the bone that typically occur in the shins and feet of runners. It can be caused by overdoing an activity before your body becomes adjusted. Pain from stress fractures gets worse with high activity but subsides with rest.
- Shin splints: This is pain that occurs on the front or inside of the lower leg and shin bone. This is common when changing a workout routine too quickly, such as increasing mileage or the number of days that you run.
- Achilles tendonitis: This is characterized by inflammation of the achilles tendon and is usually caused by repetitive stress. Other causes include adding too much distance to a running routine or tight calf muscles. It causes pain and stiffness, especially in the morning or with high activity. http://www.footankleinstitute.com/achilles-tendinosis-symptoms-and-treatment
- Muscle strain: A small tear in the muscle that is often caused by overstretching during an activity. This is common in the hamstrings, quads, calf, and groin muscles. You may sometimes hear or feel a popping sensation with this type of injury.
- Ankle sprain: An accidental stretching or tearing of ligaments around the ankle, often occurring from twisting or rolling the ankle while running.
- Plantar fasciitis: Small micro-tears occur in the tissue that runs along the bottom of the foot, causing inflammation and pain. Contributing factors include tight calf muscles and high or flat arches.
- Iliotibial band syndrome: The iliotibial (IT) band runs along the outside of the thigh and knee. When this ligament thickens and rubs the knee bone, it causes pain and inflammation.
- Patellar tendonitis
The treatments for most of these injuries is the same. Allow your body to rest, ice the area, compression and elevation, and stretch and strengthen the muscles that support the joints.
Tips to avoid running injuries: http://www.runnersworld.com/injury-prevention-recovery/how-to-prevent-common-running-injuries):
- Don’t ignore pain that doesn’t get better with rest
- Warm up and stretch before participating in any activities http://www.active.com/running/articles/the-best-warm-up-exercises-for-runners
- Add weight training and core strengthening to your routine
- Cross train—try adding some lower impact activities to your routine such as swimming or cycling
- Wear appropriate shoes
Common Injuries of a Runner
Common Injuries of a Runner
- Runner’s knee: A common overuse injury that results from the kneecap being out of alignment. Often, the cartilage on the kneecap wears down and can cause pain, particularly when going up or down stairs, squatting, or sitting with the knee bent for extended periods of time.
- Stress fractures: These are small cracks in the bone that typically occur in the shins and feet of runners. It can be caused by overdoing an activity before your body becomes adjusted. Pain from stress fractures gets worse with high activity but subsides with rest.
- Shin splints: This is pain that occurs on the front or inside of the lower leg and shin bone. This is common when changing a workout routine too quickly, such as increasing mileage or the number of days that you run.
- Achilles tendonitis: This is characterized by inflammation of the achilles tendon and is usually caused by repetitive stress. Other causes include adding too much distance to a running routine or tight calf muscles. It causes pain and stiffness, especially in the morning or with high activity. http://www.footankleinstitute.com/achilles-tendinosis-symptoms-and-treatment
- Muscle strain: A small tear in the muscle that is often caused by overstretching during an activity. This is common in the hamstrings, quads, calf, and groin muscles. You may sometimes hear or feel a popping sensation with this type of injury.
- Ankle sprain: An accidental stretching or tearing of ligaments around the ankle, often occurring from twisting or rolling the ankle while running.
- Plantar fasciitis: Small micro-tears occur in the tissue that runs along the bottom of the foot, causing inflammation and pain. Contributing factors include tight calf muscles and high or flat arches.
- Iliotibial band syndrome: The iliotibial (IT) band runs along the outside of the thigh and knee. When this ligament thickens and rubs the knee bone, it causes pain and inflammation.
- Patellar tendonitis
The treatments for most of these injuries is the same. Allow your body to rest, ice the area, compression and elevation, and stretch and strengthen the muscles that support the joints.
Tips to avoid running injuries: http://www.runnersworld.com/injury-prevention-recovery/how-to-prevent-common-running-injuries):
- Don’t ignore pain that doesn’t get better with rest
- Warm up and stretch before participating in any activities http://www.active.com/running/articles/the-best-warm-up-exercises-for-runners
- Add weight training and core strengthening to your routine
- Cross train—try adding some lower impact activities to your routine such as swimming or cycling
- Wear appropriate shoes
Pes Planus - Causes & Treatment for Flat Feet
Pes Planus - The Causes and Treatment for Flat Feet
Pes planus is a common issue that is easily diagnosed, and one we treat often. It is a condition in which the arch of your foot is lowered or flattened out, which causes excessive pronation of the foot, forefoot abduction, and eversion of the heel, as seen in the video below.
In most people with flat feet, the inside edge of their shoes typically wears down more quickly because their weight is on the inside of their foot. While most patients know what flat feet are, most don’t know what causes it or why we need to treat it because most of the time it is a painless condition.
Pes planus can be inherited or can be caused by the arches not developing during childhood. It can also be acquired over time, caused by conditions such as rheumatoid arthritis, stroke, diabetes, obesity, hypertension, or from simple wear and tear stresses of age that weaken the tendon that runs along inside of ankle and helps support your arch. http://www.footsmart.com/health-resource-center/foot/flat-feet-fallen-arches
Most patients rarely have symptoms, but pes planus could cause pain in the foot because of changes in work environment, injury, sudden weight gain, activities that put excessive stress on the feet (excessive standing, walking, jumping, or running), or footwear with limited support. This pain can be relieved with calf stretching or foot strengthening exercises, over the counter medications, heat therapy or massaging. Flat feet can alter the alignment of the legs and could cause instability, or even ankle, knee, or lower back joint issues.
Treatment for children with flat feet is typically straightforward because their feet are flexible, meaning their foot is mobile but has excessive valgus at the heel http://medical-dictionary.thefreedictionary.com/calcaneal+valgus and minimal arch height when the child is weight bearing. This is typically able to be corrected with good shoes and foot orthotics to realign the arch and give added stability. However, treatment in adults can be more complicated.
Adult Acquired Flatfoot
Adult acquired flatfoot over time and can be classified into 4 different stages:
- Stage I: pain along the medial ankle and arch with bilateral symmetrical flatfoot. This can be treated with custom foot orthotics and well-fitting shoes with good support. The purpose of orthotics is to block or limit painful or destructive motion without reducing or restricting normal motion or muscle function. Physical therapy should be used in stage I or early in stage II to strengthen the muscles and tendons that help support your arch.
- Stage II: divided into 5 sub-stages in which the deformity gets progressively less flexible. The deformity is also no longer symmetrical. Early in stage II, foot orthotics may be able to correct some of the deformity, but as you progress to late stage II, a short ankle foot orthotic (AFO) may better control the foot and ankle. The device should be articulating, allowing normal motion at the ankle, while still supporting the arch and maintaining the ankle in a neutral position. (http://www.podiatrytoday.com/addressing-biomechanics-stage-ii-adult-acquired-flatfoot)
- Stage III: the deformity is now completely rigid with a flat foot and valgus at the heel. This deformity needs increased control, so your orthotist may recommend an ankle gauntlet type AFO that is non-articulating. A rocker sole may also be added to your shoe to aid in rollover while you are walking since there is no movement at the ankle.
- Stage IV: characterized by arthritis and a valgus deformity at the ankle. Typically the best treatment for late stage III or stage IV flat foot is a solid ankle AFO or surgical treatment.
Certain modifications can be made to your orthotics to better support your flat feet.
Living With Diabetes: Diabetic Foot Care Tips
Living With Diabetes: Diabetic Foot Care
Two of the most important things you can do if you are diabetic are control your sugar and take care of your feet. Diabetes can cause a loss of sensation in your feet, which means you could step on something or a callus could form and you wouldn’t know unless you take the time to look at your feet. It can also cause limited blood flow, which complicates and lengthens the healing process.
Foot Care Tips
Those with diabetes also may have poor immune systems and can be more susceptible to infections. Left unchecked, calluses and injuries can lead to infected ulcers and ultimately to amputation. The good news is that amputation can be prevented by following these foot care tips.
- Check your feet daily: At the end of the day when you take your shoes off, inspect your feet. (http://www.webmd.com/diabetes/video/kahn-diabetes-patients-must-check-feet)If you are not able to see the bottom of your feet, use a handled mirror. If you see any skin breakdown, including blisters or ulcers, stay off your feet and make an appointment to see you doctor. Continuing to walk on even small injuries can lead to larger injuries and wounds that are difficult to heal.
- Early treatment: if you discover a wound on the bottom of your foot, see a doctor immediately to check for infection. If there is an infection, treatment with antibiotics is typically successful in early stages. If you continue to wait and walk on the wound, the infection could worsen and cause gangrene or bone infection.
- Wear proper shoes and footwear: Diabetic shoes are extra deep and extra wide to protect your feet from pressure, and don’t have seams on the inside that cause friction. They also allow room for diabetic foot orthoses, which distribute pressure over the entire foot, preventing pressure points that may lead to skin breakdown. It is also a good idea to wear seamless, padded, moisture-wicking socks. (https://www.drcomfort.com/our-footwear)
- Charcot: if you notice the shape of your arches changing, along with heat and redness at the arch, you may have a condition called Charcot, in which the bones of your feet break down. Left untreated, this can cause major deformity, which may lead to skin breakdown.
If you experience these symptoms, set up an appointment with your doctor. They may recommend that you get a brace to help support your arch and prevent further breakdown and deformity. - Keep your skin dry: infections thrive in moist environments, so allow your shoes to air out and wear socks that wick away moisture.
- Avoid going barefoot: wearing shoes will help prevent you from stepping on debris or getting small cuts and scrapes on your feet that could lead to infection.
- Keep your nails clean and short: A fungal infection causes thickening of the toenails, and pressure on the top of the nail could lead to ulcers underneath, which are difficult to spot and treat and may lead to infection. (https://www.healthstatus.com/health_blog/diabetes-3/diabetic-nail-care/)
- Be careful of water temperature: when taking a bath, check the water temperature with your arm before stepping in. If you have loss of sensation in your feet, it’s easy to step into a bath and not realize you are actually burning your skin, which could leave you susceptible to infection.
If you are diabetic, it is extremely important to follow these tips to stay healthy and prevent any complications. Get into a regular routine of non-impact exercise, stop smoking, keep your sugar controlled, and get regular check-ups.
Proper Shoe Fit - Avoiding Foot Pain, Bunions and More
Proper Shoe Fit
Buying shoes that fit well is essential to good foot health. Poorly fitting shoes can lead to pain, bunions, corns, calluses, hammertoes, plantar fasciitis, and even stress fractures. But how do you know if you’re buying the right shoes? Do you need a bigger size, a different style, or a wider shoe? Picking out shoes can be a daunting and overwhelming task, but these tips can help to point you in the right direction.
We tend to see a lot of patients who are convinced they wear a certain size, then when we measure their foot it ends up being a size or more smaller than they expected. It’s easy to forget when you’re buying shoes that they come in different widths, not just different sizes. While getting a larger size will help the shoe to fit better, it also lengthens the shoe and could cause you to trip over your toes when you walk.
Brannock Device
One way to know what size and width to start with is having your feet measured with something called a Brannock Device:
These measure both the length and the width of your foot, and most stores that sell shoes will have one of these on the sales floor. Most people have one foot that is slightly larger than the other foot, so make sure to buy shoes according to the size of your larger foot. Have your feet measured at the end of the day—as we stand and walk throughout the day, our feet swell. Measuring your feet and buying shoes at the end of the day ensures that you will be comfortable all day, not just when you leave first thing in the morning. Every shoe company makes their shoes using different lasts (or molds), (http://www.shoeschool.com/shoeschool/lasts/shoe_lasts_what.html) there may be a slight variation in sizes between companies, so while the measured size may not be the exact size you get in every single shoe, it will give you a good starting point. In addition, have your feet measured each time you buy shoes. Our feet change shape and size as we get older, so you may need a different size now than you bought last time.
How to get the right fitting shoe
One of the great myths of buying shoes is that you should give them time to “stretch out”. Don’t buy shoes that are tight or uncomfortable and expect them to stretch to fit to your foot. Your shoes should feel comfortable and fit well in the store. Bring the socks you typically use for walking or running to try on shoes. Take a few laps inside the store to ensure that your heel does not slip out of the shoe and that there is no chafing anywhere inside the shoe. When you stand, there should be about 3/8” to ½” between the end of your longest toe and the end of the shoe. (http://sizeadvisors.com/blog/2011/11/29/what-experts-can-tell-you-about-toe-allowance-part-1/)
Differences Between Walking Shoes, Running Shoes, and Other Types of Shoes
Make sure to also match the shoe to the activity you will be doing.
There are differences between walking and running shoes, or between trail running and hiking shoes. Running shoes typically have a slightly higher heel than a walking shoe due to where foot contact with the ground occurs (http://www.newbalance.com/article_walking_vs_running_shoes.html) good shoe construction consists of a cushioned heel, especially for high-impact activities such as running and jumping; a firm sole that doesn’t twist or bend easily, to give increased support especially on uneven terrain; flexibility at the proper area for the activity you will be doing; proper arch support; and a soft, breathable upper section to match the shape of your foot.