What Is Plantar Fasciitis?
Plantar fascia is the tissue that connects the bones on the bottom of your feet. It stretches the entire length of your foot, from heel to toes, and acts with the muscles in the foot and leg to hold the shape of the arch.
Normally, the fascia acts as a shock absorber, stretching each time you take a step. Placing increased forces on the foot over time can lead to an overuse injury; tiny micro-tears occur in the tissue, causing irritation and inflammation. This issue is common in runners or people who spend significant amounts of time on their feet for their job.
Symptoms
Typically, plantar fasciitis will present as pain in the foot, especially with pain in the arch or heel. Most patients complain that their heel pain is worse when they take their first few steps in the morning, and describe it as a burning or stabbing sensation on the bottom of their feet.
Causes and Contributing Factors of Plantar Fasciitis
There is no clear cause for plantar fasciitis, but studies have revealed several risk factors that could be contributing to the issue. These include:
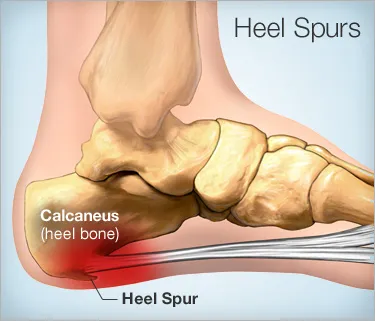
- –Bone spurs at the heel (heel spurs): Bone spurs are calcium deposits on the underside of the heel bone that can further aggravate the plantar fascia
- –Flat feet, overpronation, or high arches: As seen in the picture below, differences in the arches cause the plantar fascia to change shape, which in turn causes increased stress and inflammation to the tissue
- –Tightness in the calves or Achilles: The Achilles tendon and the plantar fascia both attach to the heel bone, as depicted below. When the Achilles tendon or calf muscle is tight, it pulls the heel upward, stretching the plantar fascia and causing inflammation.
- –Weight gain: Weight gain increases the forces placed on the feet and plantar fascia while you walk, which causes the tissue to stretch more than normal and could cause the micro-tears associated with plantar fasciitis.
- –Abnormal anatomy or walking pattern: Similar to the effects different arch shapes have on the plantar fascia, any change in the boney anatomy of the foot can change the shape of the plantar fascia and contribute to pain in the foot.
- –Wearing improper shoes: Wearing shoes with high heels can cause a tight calf muscle, which, as mentioned earlier, can be a risk factor for plantar fasciitis. Additionally, wearing shoes that have limited shock absorption can place more stress on the plantar fascia and contribute to increased pain and inflammation.
- –Overdoing certain physical activities: Activities such as running, jumping, climbing, and dancing cause excessive forces on the feet, which is absorbed by the plantar fascia and can lead to injury and inflammation.
Chronic conditions such as arthritis and diabetes have also been shown to increase risks of plantar fasciitis.
Plantar Fasciitis Treatments
Take a Load Off—Options for Treating Plantar
There is no “cure” for plantar fasciitis, but there are several ways you can limit the pain to help your plantar fascia heal:
- –Rest– Try to stay off your feet and elevate them for about 20 minutes twice a day.
- –Ice– Ice your feet for about 20 minutes at a time. If you ice multiple times per day, give your feet at least an hour between sessions. (https://heelthatpain.com/icing/) You can use gel ice therapy slippers or a typical ice pack. Additionally, you can freeze a water bottle and roll your foot over it to combine stretching and icing. You can alternate with heat therapy as well.
- –Stretch– Do the stretches shown in the video below for at least 30 seconds at a time. You can also roll a tennis ball under your foot for 3-5 minutes to help stretch the plantar fascia. Lastly, you can talk to your doctor about a night splint to stretch your heel while you sleep.
http://www.healthline.com/health/fitness-exercise/plantar-fasciitis-stretches#Stretching2
–Shoes and inserts— Try to wear supportive shoes with good shock absorbency; don’t go barefoot. Inserts can help as well, by supporting your arch and correcting foot and ankle alignment, as well as providing some additional shock absorption.
What Can an Orthotist Do for You?
Your doctor may suggest either a night splint or orthotics to decrease pain from plantar fasciitis, both of which can be provided by an orthotist. They can fit you with a night splint, which holds your ankle at 90 degrees while you sleep to provide passive stretching of your calf muscles. (http://www.plantarfasciitisresource.com/best-plantar-fasciitis-night-splint/) They can also provide either off the shelf or custom orthotics, which will provide increased support for the arch and redistribute the pressure on your feet while you walk to help with your heel pain. Orthotics can also correct your foot and ankle alignment to decrease forces on your plantar fascia, and can act as a shock absorber while you walk.