Volume Management
There are many factors that can affect volume of a residual limb.
Muscle atrophy, weight changes, diet, medication, and increased or decreased physical activity can all have significant effects. Managing these volume changes is important to ensure a well-fitting socket, which will increase stability and comfort when walking.
- After amputation surgery, we encourage our patients to wear a shrinker for about 2 weeks prior to casting. This helps to reduce postoperative edema (swelling) in the residual limb and will aid in shaping the limb for comfortable prosthetic fitting. Elevating the limb will also help to reduce swelling.
- After delivery of the prosthesis, we still want to manage volume as it can change from day to day, from morning to afternoon, and even from hour to hour. Socks are an excellent way to maintain a snug fit in your prosthesis.
- If you experience significant volume changes from day to day, keep a log of your diet and medications to show to your physician. Eating a salty meal will cause your body to retain water, which could increase volume in your residual limb. Certain medications can cause your body to increase or decrease water retention as well.
- Dialysis can have a significant affect on residual limb volume. Make sure your prosthetist is aware of when and how often you have dialysis as this can affect fitting of a prosthesis.
- Increased physical activity will most likely reduce your volume. When you put weight on your prosthesis, there is a pumping action of the muscles that will push the fluid out of your limb. You will most likely need to add socks if you are doing a significant amount of walking or going to the gym.
- Sitting with your leg hanging off a chair will increase volume. If you are sitting, elevate your limb to prevent fluid collection.
- Weather can affect volume as well. Heat can cause increased swelling, and high or low-pressure systems accompanying storms can affect your limb as well, affecting volume and sometimes increasing phantom limb type sensations.
If you are concerned about volume fluctuations or feel like adjustments need to be made to your prosthesis, call your prosthetist for an appointment.
Sweat
“How do I stop sweating so much?”
This is one of the questions we hear most often from our amputees.
Unfortunately, sweat is something that, to a certain degree, is going to happen no matter what. Most liners are made of a gel material, which retains heat and will not wick moisture away from your limb.
Excess sweat can cause several issues when using a prosthesis.
First, excess sweat can cause friction between your liner and your skin, which could lead to the formation of blisters. Blisters can take a long time to heal, and if they burst can become infected.
If blisters or other skin breakdown occurs, your physician or prosthetist may suggest not wearing the prosthesis and staying off your feet for a few days to allow it to heal.
Secondly, excessive sweat buildup in the liner can cause the liner to slide on the skin.
This can affect suspension on your leg, and can cause shear forces which can lead to skin breakdown. Luckily, there are a few tips and tricks to managing and reducing the effects of sweat on your residual limb.
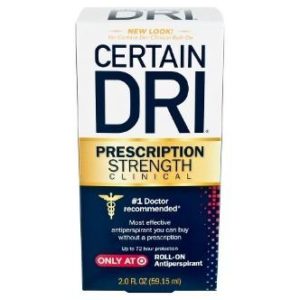
Antiperspirants — There is a specific antiperspirant that we have found works very well for our patients called Certain Dri. It can be found in most drug stores and does not require a prescription.
The important thing to remember when searching is to find an antiperspirant, not a deodorant. We typically suggest that our patients put Certain Dri on their limb at night after taking the liner off and cleaning their leg. After about 2 weeks of using this, our patients are typically seeing a dramatic reduction in sweat.
Note: start on a small section of skin first to ensure that you will not have any adverse reactions.
Liner liner — This is a very thin sock that goes between your leg and your liner. It will help to wick away moisture and reduce shear forces, which could cause skin breakdown.
Most liner liners will have silver fibers to help eliminate odors as well.
Suspension — There are certain types of suspension that can help reduce sweating, specifically vacuum suspension.
An active pump in the prosthesis maintains negative pressure in the socket, meaning the limb will always be in close contact with the gel liner, preventing sweat glands from generating excessive moisture.
What NOT to do
It is easy to be tempted to put baby powder or talc powder inside the liner to help absorb moisture.
However, the powder will just absorb the sweat and become a sticky paste inside the liner, making it uncomfortable and difficult to clean out. Additionally, using lotion before putting the liner on can increase the detrimental effects of sweat, such as skin breakdown or causing the liner to slide down your leg.
We typically encourage people to use lotion at night after cleaning their leg to allow time for the lotion to absorb into the skin. If you use lotion, use a non-scented lotion that is gentle on skin. Scented lotions can easily cause skin irritation, especially inside a hot and sweaty liner.
If you feel like you are having an issue with sweat, try these tips or speak to your prosthetist to find a solution specific to your needs.